That’s what happens to your fat cells when you put on weight
If you’re overweight or have developed a paunch, you’re probably suffering from chronic inflammation of your adipose tissue. This is a silent pathological process which sooner or later will become a ticking time bomb, so it makes sense to read up on the latest findings and take action fast.
What happens when you put on weight?
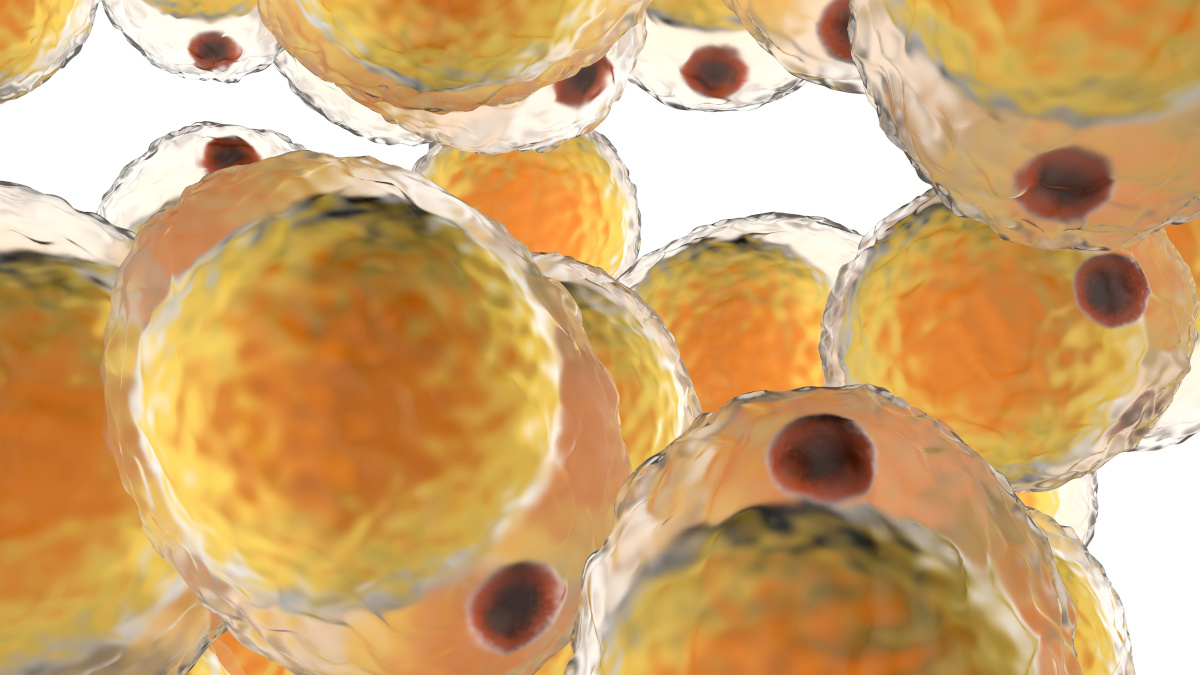
Gaining weight is an entirely natural process – it’s the means by which energy which is surplus to immediate requirements is stored for future use. In this way, there is never any waste and the body is able to survive periods of food scarcity without difficulty. Unfortunately, what was a blessing for our ancestors has turned into a veritable curse in today’s affluent societies. Decreased levels of physical activity, an abundance of foodstuffs and the calorific nature of that food have all interfered with this mechanism and led to an epidemic of excess weight.When a person becomes overweight, it’s because their calorie intake has exceeded their energy output for a certain period of time: the surplus energy has therefore been stored in specialized cells called adipocytes. It is these cells which primarily make up adipose tissue, the soft tissue responsible for unsightly bulges. Energy reserves are stored in the form of lipids: they penetrate the adipocytes which inflate like balloons as the fats accumulate.
If the calorie/energy imbalance persists, the adipose tissue continues to expand, forcing the body to recruit yet more fat cells and to reconfigure blood flow pathways in order to feed them properly. But if the adipocytes grow too large, they end up becoming oxygen-deficient and they suffocate: the blood vessels are no longer able to reach them and the oxygen diffusion distance may be exceeded (2-3).
This lack of oxygen, or hypoxia, creates chaos in adipose tissue.
- It causes chronic inflammation of adipose tissue.
This same inflammation travels towards the bloodstream where it can be measured using a specific test. With it comes a massive infiltration of macrophages. These primitive immune cells are attracted by certain cytokines (especially MCP-1) secreted by the suffocating adipocytes. - It results in the formation of collagen deposits which trap the adipocytes.
Inflammation of adipose tissue is accompanied by deposits of type VI collagen which make the tissue stiff and fibrous (4-5). Fibrous bands form in the extracellular milieu which prevents the adipocytes from expanding and storing more excess lipids. They are instead redirected towards vital organs such as the liver, muscles and heart, so increasing the accumulation of fat deposits in undesirable places. And it is precisely this redirection of fats which is responsible for many health problems including cardiovascular disorders, resistance to the pancreatic hormone, type 2 diabetes and hepatic steatosis (fatty liver) (6). - It makes losing weight more difficult. As has been shown in several studies, the more a person’s fatty tissue has been subject to fibrosis, the harder they will find it to lose weight. Which is why this pathological process may well turn out to be a potential target in the treatment of obesity (7-8)!
How do you know if your body fat is normal?
According to scientists, fibrosis of fatty tissue does not just occur in obese individuals. It can also develop in slim people with very little fat under the skin, but who have a ‘potbelly’ or are ‘apple-shaped’. In such individuals, fat is deposited in the abdominal area, in the innermost layers of the stomach around the internal organs. This particular pattern of fat accumulation is especially dangerous to health.Fat is deposited at several main sites in the body: subcutaneous tissue, visceral tissue, around the hips and around organs such as the heart and kidneys. Each of these types of fat deposit has a specific hormonal profile, ie, they do not all secrete the same messengers and do not, therefore, lead to the same consequences if the deposits get bigger or become problematic. For example, fat deposited in subcutaneous tissue does not appear to be linked to obesity, whereas that deposited in visceral tissue seems to be particularly vulnerable to fibrosis (10).
How do you know if you should be worried about your abdominal fatty tissue? To be certain, you’d need to measure your inflammation levels and identify whether or not fibrosis has taken place. A simpler guide is whether or not you feel too fat in the abdominal area, although this is not necessarily indicative, since slim people can be affected while obese individuals remain ‘metabolically healthy’ (11). How you feel, what your body’s telling you, whether you’re suffering from inflammation problems or fatigue and if you’re finding it difficult to lose weight (even if you’re not significantly overweight) are all vital clues.
What happens if you do nothing?
It should be stressed that fatty tissue is not simply a facility for storing fat: it’s an organ which secretes numerous chemical messengers (in particular, leptin and adiponectin) which have a direct effect on the body as a whole - the immune response, blood pressure, haemostasis, regulation of bone mass, food intake, functions controlled by the thyroid and even reproduction. In other words, if your fatty tissue has been affected by fibrosis, it’s your whole body that suffers.It therefore requires urgent action in order to prevent the threat of type 2 diabetes or atherosclerosis. The longer you wait, the more likely it is that fibrosis will develop and cause overall degeneration of tissue. Following are five steps to consider right now if you want to reduce your fatty tissue and inflammation levels:
- Physical activity is the crucial element in getting rid of visceral fat. It is essential for increasing and maintaining muscle mass which is often greatly diminished.
- Several studies have shown that secretion of the hormone cortisol (excess levels of which are produced in chronic stress) is associated with an increase in abdominal fat (12). It’s therefore important to do all you can to take time to relax and try to achieve greater serenity in your life.
- The recruitment of fat cells is exacerbated by dietary factors such as an unbalanced intake of omega-6 and omega-3 fatty acids. So ensure you lower your intake of omega-6 (found in a great many processed foods) and increase that of omega-3.
- Achieving weight loss inevitably means eating a lower-calorie diet. It’s therefore important to ‘stay the course’ and to use complementary strategies, be they psychological or nutritional, to help you do so (for example, taking natural-source appetite-suppressants, such as Appetite Control Formula or CSAT).
- Consider products specifically formulated to inhibit the formation of fat cells such as Adipromin® or those designed to get rid of visceral fat such as Advanced Fat Burner. Remember that probiotics can help in addressing excess weight and inflammation. Research has shown that gut flora plays a key role in controlling visceral fat and inflammation: bacterial strains such as Lactobacillus gasseri and Lactobacillus reuteri can help fight inflammation and excess weight.
SuperSmart ADVICE
References
- Pasarica et al. Reduced adipose tissue oxygenation in human obesity: evidence for rarefaction, macrophage chemotaxis, and inflammation without an angiogenic response. Diabetes. 2009 Mar;58(3):718-25. doi: 10.2337/db08-1098. Epub 2008 Dec 15.
- Ye J, Gao Z, Yin J, He Q 2007. Hypoxia is a potential risk factor for chronic inflammation and adiponectin reduction in adipose tissue of ob/ob and dietary obese mice. Am J Physiol 293: E1118–E1128 doi: 10.1152/ajpendo.00435.2007
- Khan T, Muise ES, Iyengar P, Wang Z V, Chandalia M, Abate N, et al. Metabolic dysregulation and adipose tissue fibrosis: role of collagen VI. Mol Cell Biol 2009;29:1575–91. doi:10.1128/MCB.01300-08.
- Sun K, Kusminski CCM, Scherer PEP. Adipose tissue remodeling and obesity. J Clin Invest 2011;121:2094–101. doi:10.1172/JCI45887.2094.
- Muir LA, Neeley CK, Meyer KA, Baker NA, Brosius AM, Washabaugh AR, et al. Adipose tissue fibrosis, hypertrophy, and hyperplasia: Correlations with diabetes in human obesity. Obesity 2016;24:597–605. doi:10.1002/oby.21377.
- Alkhouli N, Mansfield J, Green E, Bell J, Knight B, Liversedge N, et al. The mechanical properties of human adipose tissues and their relationships to the structure and composition of the extracellular matrix. AJP Endocrinol Metab 2013;305:E1427– 35. doi:10.1152/ajpendo.00111.2013.
- Fried SK, Moustaid-Moussa N. Culture of adipose tissue and isolated adipocytes. Methods Mol Biol 2001;155:197–212. doi:10.1385/1-59259-231-7:197.
- Takaoka M, Nagata D, Kihara S, Shimomura I, Kimura Y, Tabata Y, Saito Y, Nagai R, Sata M. Periadventitial adipose tissue plays a critical role in vascular remodeling. Circ Res. 2009 Oct 23;105(9):906-11. doi: 10.1161/CIRCRESAHA.109.199653. Epub 2009 Sep 17.
- Samaras K., Botelho N.K., Chisholm D.J., Lord R.V. Subcutaneous and visceral adipose tissue gene expression of serum adipokines that predict type 2 diabetes. Obesity. 2010;18:884–889
- Carnethon MR1, De Chavez PJ, Biggs ML, Lewis CE, Pankow JS, Bertoni AG, Golden SH, Liu K, Mukamal KJ, Campbell-Jenkins B, Dyer AR. Association of weight status with mortality in adults with incident diabetes. JAMA. 2012 Aug 8;308(6):581-90. doi: 10.1001/jama.2012.9282.
- Brunner EJ, Chandola T, Marmot MG. Prospective effect of job strain on general and central obesity in the Whitehall II Study. Am J Epidemiol. 2007;165:828-837.
Keywords
3 Days
My skin is clearing up nicely!
Pretty good for my skin so far.
Christian
6 Days
The new packaging is excellent
The new packaging is excellent - finally! No more squashed boxes and torn envelopes.
GORAN
6 Days
Great Product
Great Product
Larry Garrett
11 Days
Quick shipping
Quick shipping; good price. No issues!
Mary McCarty
12 Days
Thr product is very good and is helping…
Thr product is very good and is helping me on my health. Then is always on time
LUGO Luz
15 Days
Buying was fine
Buying was fine. I had problems with the website not recognizing my login info, and had to call to get it fixed. Other than that, everything was good.
David S. Clark
15 Days
Your super maca and super ginseng are…phenomenal
Your super maca and super ginseng are phenomenal supplements that compliment each other when taking them together. Fantastic feeling of well-being and lots of mid day energy without the crash.
Keith Mason
18 Days
I have had amazing results with every…
I have had amazing results with every supplement I've purchased. I am extremely satisfied with this company
kirstin Torres
18 Days
Fine products
Fine products . They are on the leading edge of online supplements. The only issue -so far-is they sometime run out of subscription items.
Jason Argos
21 Days
The ordering process is very user…
The ordering process is very user friendly and the products always come in a timely manner.
CARTER Rhonda
22 Days
The price for Dr
The price for Dr. Pero's AC-11 is reasonable and in line with his views. (my former colleague). Keep it pure.
CAMPBELL Clayton
24 Days
Right on every time.
Right on every time.
Arthur Nicholas
27 Days
They are cheaper than everyone else and…
They are cheaper than everyone else and the shipping was fast. Great company.
Patricia Adams
34 Days
Availability of quality health…
Availability of quality health supplements and it's wide variety is impressive. Ordering is seamless and shipping even during the holidays is well streamlined.
Mohamad Hussein
48 Days
A Product worth waiting for when not…
A Product worth waiting for when not available and then arriving as a surprise!
DOMINIC